* lab name Z-0 [mB/1] (patent pending)
Freeing life for the eyes!
The Sloboda Clinic, Zagreb, Croatia, is embarking on a final stage of clinical trials for a groundbreaking new treatment for blindness that has been the subject of intense research for over two decades. Our emerging results are encouraging and indicate that we have refined the necessary factors to enable a total cure of all forms of blindness in mammals.
Registration is currently open to blind participants who want to contribute to medical research. Please follow the links on this site for further information.
Our staff

Our highly trained team of over four internationally trained Ophthalmic consultants, doctors, nurses and researchers are based at the Sloboda Clinic which is headed up by Professor Goran Cudo.
Professor Cudo is a consultant Ophthalmologist and Eye research specialist who has worked in Zagreb since 1999. He specialises in laser eye surgery, vitreoretinal surgery and cutting edge bubble-based therapy.
He was recently cited by a leading Balkan medical journal as one of the region’s top 100 Consultants, in recognition of his groundbreaking work in Ophthalmology.
He says: “I go to bed at night with the dream of helping people do more with their eyes and their lives”
1985 – Degree in Medicine at The University of Zagreb Medicinski fakultet School of Medicine
1989 – PhD in Opthamology from Harvard University
Currently continuing sabbatical research at the University of Cambridge whilst also working as a senior lecturer in BioMedical sciences.
Professor Cudo, Dr Marko Huzjak and Professor Ravi J Singh were nominated for the Lasker Award in 2009 for contribution to medical science with the break-through discoveries of the action of an isomer of Oxiglil on the parasympathetic pathways in the optic chiasm.
Professor Cudo has also won the Albany Medical Center Prize in Medicine and Biomedical Research for his work on ocular regeneration.
Dr Marko Huzjak is famous for his work in functional biomaterials for medical devices, nanomaterials, and nanostructures for cell regeneration, winning the Distinguished Alumni of the Year Award from John Hopkins Medical School in 2007.
Professor Ravi J Singh provided a break-through in the treatment of caratcts, inventing a way to create ultra-thin plastic-analogue made out of the sufferers hair cells to manufacture an artificial intraocular lens implant that will not be rejected by the host. For this he was awarded the Nobel Prize for physiology in 2004.
Research
Bubble Acoustics
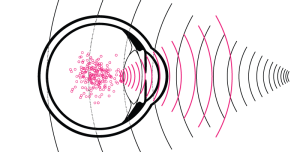
Bubble acoustics is a groundbreaking new technique utilised by Dr Cudo and his team at the Sloboda Clinic. It allows the guided transportation and delivery of drugs within the human body, by means of sound wave vibrations propagated by bubbles. The “magic ingredient” is an experimental drug commonly referred to as Fluomephil*.
This is a combination experimental drug based on the composition of “Vitreous Humour” extracted from the donated eyes of the deceased. Fluomephil will be used to regenerate ocular cell structure and tissue.
The technique has been refined by drawing on insights from Professor Cudo’s medical anthropological field studies of natural healing methods used for millennia by indigenous people in many remote parts of the world.
In short, we are combining the technology of micro gas -filled bubbles only a few nanometres in diameter (less than one hundredth the width of a human hair) – already widely used in allopathic medicine, to enhance ultrasound images – with the ancient wisdom unearthed through decades of anthropological research.
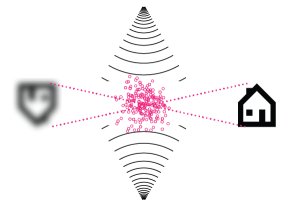
When the micro gas-filled bubbles containing Fluomephil are injected into the bloodstream, they reflect a stronger acoustic signal through their echoing vibrations than the surrounding tissue. We have exploited this technology using ultrasound waves of carefully calculated frequencies to guide and track the bubbles accurately through ocular veins to precisely the right part of the eye. The bubbles are made from lipids filled with a heavy ‘fluorocarbon’ gas, having the advantage of not dissolving easily in the blood stream, thereby ensuring the bubbles containing the Fluomephil stay intact until they reach the correct location within the eye.
The added benefit is that ultrasound can also be used as a detonator at a specific moment using a further higher frequency to explode the bubbles, causing temporary rupture of cell membranes. This helps to release the Fluomephil into the cells where it can be absorbed more effectively.
All this is administered by one simple injection to the temple and then needs a approximate 24 hour transit time for the bubbles to reach the correct location. Then with a simple trigger ultrasound pulse sent remotely via the patients headphones, the bubbles are burst the, the drug is released, and does its work almost instantaneously.
In previous trials only 20% of mice injected with the non-placebo drug showed signs of severe frontal hypothalmic dysfunction!
